What Role Will AI Play in Resource-Poor Health Care Settings?
AI could bridge disparities in health care, but certain obstacles still stand in the way
Artificial intelligence (AI) describes a range of techniques that allow computers to perform tasks typically thought to require human reasoning and problem-solving skills. Recently, with the rapid development of computers, the internet, advanced statistics, and machine learning technology, in addition to the increase in handheld and wearable networked devices such as smartphones and watches, AI technology is bringing about revolutionary changes across the health care field. While many AI applications are being rapidly deployed and imbibed into the health care systems in developed countries, their application in resource-poor or developing nations had been at a fairly nascent stage until now. However, this situation is rapidly changing.
On the disease trail
Several recent examples demonstrate how AI is helping predict, model, and slow the spread of diseases in resource-poor settings. Machine learning tools that can observe and understand patterns in data are being fine-tuned to predict the transmission of vector-borne tropical diseases based on weather and land-use patterns; for example, a Bayesian network system was recently developed that can predict dengue outbreaks a month in advance and geo-locate them within a 400-meter radius. Electronic medical records, online media, and social media are increasingly being put to use to make outbreak predictions in resource-poor settings. Global Health Monitor is one such smart tool—it helps epidemiologists and program managers monitor the spread of diseases by identifying and plotting relevant news stories on a map. Mobile health applications, such as health care guidance apps that allow users to input details of their symptoms and seek appropriate care virtually when they are unable to seek a face-to-face appointment with a physician, are becoming particularly useful in resource-poor settings where there has been strong mobile phone penetration. Increasing mobile device ownership in developing nations also means people can easily collect and monitor their own health data in real time, effectively shifting health care from the hospital to home. Mobile “smart” devices not only empower the patient but can also educate health care workers by keeping them abreast of the latest findings and knowledge in their areas of expertise, especially in remote areas where access to medical literature might otherwise be difficult.
Understaffed, overburdened
In resource-poor countries, the health care system is usually understaffed and overburdened. Hospitals suffer from poor infrastructure and a severe shortage of skilled workers. Automation of routine and straightforward tasks can free up precious human resources to allow health care workers to focus on more complex cases in which they can make a bigger difference. For example, an AI system introduced in a hospital can automate the process of measuring patients’ vital signs so that care teams can be alerted sooner to any changes in a person’s condition. These systems reduce the incidence of unexpected medical emergencies and shorten hospital stays while freeing up hospital staff to focus on patient care rather than monitoring. However, the economic situation in many developing nations might not support the implementation of such a system because the sum of the equipment, personnel, training, and transportation of AI-based diagnostics can represent a huge economic burden. Therefore, advanced AI technology solutions may prove to be too costly in these settings, at least initially. For deeper penetration into resource-poor areas, low-cost, clinical-grade smart diagnostics that are robust and low maintenance need to be developed. Such devices would be able to offset a part of the economic burden associated with advanced AI solutions.
Primary health care services
Machine learning can be applied to improve the provision of primary health care services in resource-poor settings. Immunization drives, supply chain for medicines, and referral services can be greatly improved using machine learning. For instance, Tanzania and Zambia maintain comprehensive immunization data sets in the form of electronic immunization registries, which have been instrumental in closing the immunization gaps in these countries because the data can be used by machine learning models to predict vaccine use in health facilities months in advance. These predictions effectively bridge the supply-and-demand sides of vaccines, reduce wastage, and eliminate stockouts. Greater accuracy of forecasting vaccine use leads to lower costs, more efficient use of resources, and fewer missed opportunities for vaccination. Predictions made by machine learning models can also improve inventory management and supply chain of other medications, providing similar benefits of reduced wastage and optimal inventory. AI chatbots can help nurses quickly locate a certain department’s on-call physician to refer patients to or update physicians with the right information before they visit a patient’s home.
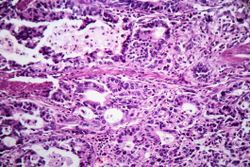
In addition to the application of AI technology in primary health settings, many AI-driven systems have been developed for special diseases. For example, a low-cost, swallowable endoscopic capsule with AI analysis technology can be used to screen for upper gastrointestinal cancers, thus replacing expensive or difficult traditional screening equipment, which may be scarce in resource-poor communities.
Advancing rural health
A serious problem in developing countries is the inequality between urban and rural health services. The shortage of qualified health care providers is the major reason for the unavailability and low quality of health care in rural areas. In addition to physicians, other health care workers—nurses and paramedical health workers—can also be trained to use AI techniques to compensate for the lack of physicians. Telemedicine powered by AI can also equip patients in remote communities to prevent and self-manage certain conditions. Introduction of computer-associated diagnostic systems in rural clinics that lack a physician has often met with positive patient responses because many patients believe that the computer system is more accurate and provides a more detailed interaction with them than do health care personnel. Mobile, all-in-one diagnostic stations, such as the one developed by WeDoctor, an internet health care startup in China supported by the national rural health care program, can independently run 11 diagnostic tests and upload data automatically for online consultation. Technology giants such as Tencent and Baidu in China and Google and IBM in Africa are collaborating with the local national health care programs and investing in AI-driven smart clinics for rural areas.
The AI obstacle course
For AI to become more powerful and relevant in resource-poor countries, certain hurdles must first be overcome. A majority of the patient data anywhere in the world today is unstructured, meaning it takes the form of physician’s notes, X-ray or MRI imaging data, patient lifestyle data, or other data that is not organized or stored in a consistent manner to enable a computer to draw meaningful conclusions. Its variable format renders unstructured data not immediately amenable to use in AI applications. The situation is worse in developing countries, where most patient data is handwritten in local languages and poorly maintained. Effective implementation of AI tools would require developing nations to invest in digital infrastructure and a common, secure system for storing patient data.
Other infrastructure issues also need to be considered; for example, although internet connectivity is improving throughout the world, some resource-poor settings remain without access to the bandwidth necessary to upload very large signal data sets to the cloud. In some developing countries, electricity might not even be available in remote locations. Overcoming the infrastructure-related hurdles would require local governments and international organizations to step in and strengthen financial support and intervene to minimize the cost of implementation of AI solutions.
While AI presents a viable and much-needed solution to doctor shortages, it introduces a demand for medical professionals who are trained in data science and AI to effectively use the AI tools at hand. A typical rural clinic in India or Africa might have a nurse with minimal training and a technician with a 12th-grade education who is not adequately skilled to provide support using advanced AI tools. The limited skill set of rural health care workers introduces the need for a user-friendly AI health care system adapted to address their needs. Initial and refresher training sessions for all health care personnel involved are critical requirements for the smooth and effective implementation of AI tools in developing nations.
Ultimately, automation of routine health care tasks and AI can go only so far in improving patient outcomes. Boosting the speed and accuracy of diagnosis is unlikely to make a difference if appropriately advanced treatment options are not available, as is the case in resource-poor settings.
The ability of AI to democratize health care around the world is one of the most exciting promises it holds. In developed nations, AI can address the widening gap between health care provision to the rich and poor. It can improve access and quality of care, which are currently hindered by poor infrastructure and skill shortages. But in order for AI to realize its potential in resource-poor settings, certain roadblocks must be overcome. Digitization of patient data, skill enhancement of health care workers, and redeployment of resources freed up by AI toward effective improvement of patient outcomes are needed for AI to realize its potential for improving health care in resource-poor settings.