Can Pharmacogenetic Testing Optimize Pain Management?
Harnessing the power of pharmacogenomics may make opioid analgesics safer and more effective
Prescriptions for opioid analgesics have nearly doubled in the United States over the past two decades.1 Yet, a proportional decrease in pain is not observed. In 2019, nearly 20 percent of US adults suffered from chronic pain and more than 7 percent had chronic pain that limited their daily activities.2 In the same year, 14,000 deaths involving prescription opioid overdose were also reported.3 In the face of this crisis, how do we optimize opioid analgesic use and dosing to provide maximum pain relief while reducing adverse effects?

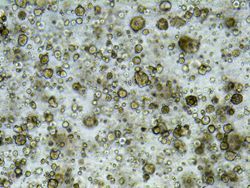
Opioid analgesics are often prescribed for the management of chronic musculoskeletal, osteoarthritis, postoperative, and cancer-related pain. However, prescription opioids exhibit significant interindividual variability in their efficacy, adverse effects, and addiction risk. Individual differences are attributed to single nucleotide polymorphisms (SNPs). SNPs may occur in genes encoding for proteins involved in nociception, drug metabolism, and efflux.
There are two underlying causes of SNP-induced variability in drug response—pharmacokinetics and pharmacodynamics. Gene variants of drug-metabolizing enzymes mediate pharmacokinetic variability. Variants of receptors and target proteins mediate pharmacodynamic heterogeneity in drug response.
Morphine and other opioid derivatives such as codeine, tramadol, hydrocodone, oxycodone, fentanyl, methadone, and buprenorphine are commonly prescribed opioid analgesics. Gene variants implicated in the diversity of opioid response are discussed below.
Genes affecting opioid pharmacokinetics
Cytochrome P450 (CYP) enzymes
Opioid analgesics are extensively metabolized by CYP enzymes in the liver and intestines.
CYP2D6 converts codeine, tramadol, hydrocodone, and oxycodone to their more potent metabolites—morphine, O-desmethyltramadol, hydromorphone, and oxymorphone, respectively. Compared with the parent drug, these metabolites have a several-fold greater affinity for μ-opioid receptors. Therefore, individuals with SNPs resulting in loss of CYP2D6 activity are poor metabolizers for each of these drugs, whereas SNPs resulting in a gain of function are rapid metabolizers. As a result, CYP2D6 poor metabolizers (individuals with CYP2D6*4, CYP2D6*17, CYP2D6*36 alleles) experience inadequate pain relief.4–6 Conversely, CYP2D6 ultrarapid metabolizers (CYP2D6*2 gene variants) produce very high concentrations of the active metabolites and are more likely to suffer adverse effects such as respiratory depression, even with low doses of the parent drug.4–6
CYP3A4 converts codeine, tramadol, oxycodone, and fentanyl to their inactive metabolites via N-demethylation. Relatively few SNPs exist on the CYP3A4 gene. The CYP3A4*1G variant (G20230A), commonly found in the Asian population, has lower activity than the wild-type enzyme. This variant has a higher analgesic response compared to the wild type, despite a lower rate of fentanyl metabolism and consumption.7,8
CYP2B6 catalyzes the conversion of methadone into its inactive metabolites. The CYP2B6*6 variant of this highly polymorphic gene is found in African, Asian, and Hispanic populations. CYP2B6*6 has reduced hepatic expression. This leads to higher steady-state concentrations of methadone, increasing the risk of serious cardiac arrhythmias and sudden death.9,10 Variant alleles also alter the maintenance dose of methadone required to treat opioid addiction.
Uridine diphosphate glucuronosyltransferase (UGT)
UGT2B7 converts morphine and hydromorphone into their inactive 3-glucuronide forms (major metabolite) and active 6-glucuronide forms (minor metabolite).
Individuals homozygous for the CC genotype of UGT2B7 802C>T tend to have higher levels of morphine-6-glucuronide compared to those with the TT genotype.11 Thus, they show an exaggerated response to even small doses of morphine, and consequently to its adverse effects.
P-glycoprotein transporter (ABCB1)
ABCB1, a transporter expressed on the blood-brain barrier, controls the access of morphine to its target site in the central nervous system. Individuals homozygous for the TT genotype of the 3435C>T SNP in the ABCB1 gene have higher levels of morphine in the cerebrospinal fluid.12 They, therefore, report greater pain relief following morphine therapy compared to CC homozygotes.13 A similar pharmacogenetic effect is also reported for fentanyl-mediated analgesia and respiratory depression.14
Genes affecting opioid pharmacodynamics
Opioid receptor mu-1 (OPRM1)
OPRM1 encodes the μ-opioid receptor—the main site of action of morphine and its derivatives. 118A>G is the most widely studied SNP on this highly polymorphic gene. The GG genotype has lower mRNA and protein expression than the AA wild type. Lower expression of the OPRM1 GG genotype and reduced binding affinity to the endogenous ligand β-endorphin may also contribute to greater pain sensitivity compared to AA homozygotes.4 Accordingly, patients homozygous for the G allele were associated with higher consumption of morphine, codeine, tramadol, and fentanyl compared to A allele homozygotes or heterozygotes.5 The 118A>G SNP, common in individuals of Asian descent, is also linked to a higher risk of opioid addiction.15
Dopamine D2 receptor (DRD2)
The dopaminergic system plays an important role in opioid addiction. The DRD2 gene is located downstream of ANKK1, a gene that encodes a serine/threonine kinase. Taq1A polymorphism in the ANKK1 gene results in lower expression and binding activity of the DRD2 protein.4 In Asian and European populations, the DRD2/ANKK1 polymorphism is associated with opioid dependence.16
Challenges in clinical pharmacogenetic testing
Although increasing evidence supports the need for pharmacogenetic testing, clinical implementation continues to languish. Currently, pharmacogenetic testing is only performed if a person is prescribed a drug that has a clinically actionable gene variant associated with it. With falling costs and rapid advances in genomic sequencing, some experts are pushing for more preemptive testing instead of a reactive approach. However, there are challenges in adopting a preemptive approach.
First, the clinical value of preemptive testing is highly contested. Several commercial multigene panels (e.g., GeneSight® Analgesic, Proove® Opioid Risk Panel, Pain Medication DNA Insight™, Millennium PGT™, and IDgenetix®) are available to aid in the prescription of opioids and pain management. However, health insurance companies still consider these tests to be “investigational.” Therefore, reimbursement is only allowed in a few strictly defined clinical scenarios, placing the economic burden of testing on the patients.
Second, there is an ongoing debate between guideline-based versus literature-based testing. The scientific literature outlines numerous gene variants capable of altering the pharmacokinetics and pharmacodynamics of opioid analgesics. However, guidelines for standardization and testing are only available for a fraction of the variant alleles.17 Guideline-based testing may omit important variants, whereas literature-based testing may be too broad to produce clinically actionable insights in diverse populations.
Lastly, health care providers have limited expertise in molecular genetics. Therefore, additional resources and support tools are required to help physicians accurately interpret and utilize pharmacogenetic test results.
Optimizing opioid therapy
Significant heterogeneity exists in individual responses to opioid analgesics. Variability in genes encoding drug-metabolizing enzymes and receptors involved in pain pathways lies at the crux of interindividual differences in opioid response. Commercial and laboratory-based tests are available to identify gene variants associated with greater consumption and a higher risk of addiction to specific opioid analgesics. These variants can help fine-tune drug doses to maximize pain relief, while minimizing adverse effects such as respiratory depression and cardiac arrhythmias. Thus, integrating standardized pharmacogenetic testing into clinical practice has the potential to optimize opioid therapy.
References:
1. Nahin, Richard L., et al. “Eighteen-year trends in the prevalence of, and health care use for, noncancer pain in the United States: Data from the Medical Expenditure Panel Survey.” The Journal of Pain 20.7 (2019): 796–809.
2. Zelaya, Carla E.,et al. “Chronic pain and high-impact chronic pain among U.S. adults, 2019.” NCHS Data Brief 390 (2020): 1–8. https://www.cdc.gov/nchs/products/databriefs/db390.htm.
3. Centers for Disease Control and Prevention. “Prescription Opioid Overdose Death Maps.” https://www.cdc.gov/drugoverdose/deaths/prescription/maps.html.
4. Nerenz, Robert D., and Gregory J. Tsongalis. “Pharmacogenetics of opioid use and implications for pain management.” The Journal of Applied Laboratory Medicine 2.4 (2018): 622–632.
5. Kumar, S., et al. “Pharmacogenetics of opioids: a narrative review.” Anaesthesia 74.11 (2019): 1456–1470.
6. Crews, K. R., et al. “Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update.” Clinical Pharmacology and Therapeutics 95.4 (2014): 376-82.
7. Ren, Z. Y., et al. “The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: a systematic review and meta-analysis.” Pain Physician 18.2 (2015): 131–152.
8. Yan, Q., et al. “Impact of CYP3A4*1G polymorphism on fentanyl analgesia assessed by analgesia nociception index in Chinese patients undergoing hysteroscopy.” Chinese Medical Journal 131.22 (2018): 2693–2698.
9. Eap, C. B., et al. “Stereoselective block of hERG channel by (S)-methadone and QT interval prolongation in CYP2B6 slow metabolizers.” Clinical Pharmacology and Therapeutics 81.5 (2007): 719–28.
10. Crettol, S., et al. “Methadone enantiomer plasma levels, CYP2B6, CYP2C19, and CYP2C9 genotypes, and response to treatment.” Clinical Pharmacology and Therapeutics 78.6 (2005): 593–604.
11. Bastami, S., et al. “Influence of UGT2B7, OPRM1 and ABCB1 gene polymorphisms on postoperative morphine consumption” Basic & Clinical Pharmacology & Toxicology 115.5 (2014): 423–31.
12. Meineke, I., et al. “Pharmacokinetic modelling of morphine, morphine-3-glucuronide and morphine-6-glucuronide in plasma and cerebrospinal fluid of neurosurgical patients after short-term infusion of morphine.” British Journal of Clinical Pharmacology 54.6 (2002): 592–603.
13. Campa, D., et al. “Association of ABCB1/MDR1 and OPRM1 gene polymorphisms with morphine pain relief.” Clinical Pharmacology and Therapeutics 83.4 (2008): 559–66.
14. Park, H. J., et al. “Genetic polymorphisms in the ABCB1 gene and the effects of fentanyl in Koreans.” Clinical Pharmacology and Therapeutics 81.4 (2007): 539–46.
15. Crist, R. C., et al. “A review of opioid addiction genetics.” Current Opinion in Psychology 27 (2019): 31–35.
16. Deng, X. D., et al. “Association between DRD2/ANKK1 TaqIA polymorphism and common illicit drug dependence: evidence from a meta-analysis.” Human Immunology 76.1 (2015): 42–51.
17. Pratt, V. M., et al. “Recommendations for clinical CYP2D6 genotyping allele selection: A joint consensus recommendation of the Association for Molecular Pathology, College of American Pathologists, Dutch Pharmacogenetics Working Group of the Royal Dutch Pharmacists Association, and European Society for Pharmacogenomics and Personalized Therapy.” The Journal of Molecular Diagnostics S1525-1578(21)00164-1.